What is a growth factor? Definition
It is a naturally occurring substance that simulate the growth of cells. It also promotes healing, proliferation, and cellular differentiation.
It acts as a signalling molecule between the cells. Growth factor is a subset of cytokines. It can be secreted by neighboring cells as well as distant glands and tissues. (3)
How growth factor stimulates growth?
Growth factors stimulate growth through the endocrine, autocrine, and paracrine mechanisms. Growth factors bind their receptors on the target cells’ surface.
However, there are a few factors that could affect the growth of target cells such as the type of receptors, transduction of intracellular signal, number of target cells, the binding ability of growth factor to extracellular matrices, growth factor concentration, and extracellular matrices degradation. (2, 4)

Photo 1: A pathophysiologic presentation of growth factors.
Picture Source: www.hgh-pro.com

Image 2: Growth factor serum, one of the popular growth factor supplements today.
Picture Source: www.dermacaredirect.co.uk
What are growth factors types?
Insulin-like growth factor 1 (somatomedins)
It stimulates cellular growth by mediating the secretion of growth hormone from the pituitary gland. It is abundant in the body following birth and play a very important role in the formation of proteins.
Epidermal growth factor (EGF)
it promotes growth of the epithelial cells.
Platelet derived growth factor (PDGF)
It stimulates the growth of muscle and connective tissue cells.
Vascular endothelial growth factor (VEGF)
Stimulates the blood vessel formation
Nerve growth factor (NGF)
It stimulates the growth of neuronal cells
Erythropoietin
It stimulates the growth of red blood cells. It also plays a very important role in the treatment of anemia secondary to chronic kidney failure.
Granulocyte colony stimulating factor (GCSF) and granulocyte macrophage colony stimulating factor (GMCSF)
They stimulate the production of white blood cells in patients with cancer.
Fibroblast growth factor (FGF)
They are primarily involved in embryonic development, wound healing, angiogenesis, and endocrine signalling pathways.
Growth Factor Classes
- Class I – These are growth factors that interact with a particular type of receptor at the surface of the cell. Examples of class I growth factors are platelet derived growth factor (PDGF), epidermal growth factor (EGF), and growth hormone (somatotropin).
- Class II – They are cell surface hormone receptors.
- Class III – They are a large group of intracellular signal transmitters.
- Class IV – They are proteins that bind to the specific DNA segment or also called nuclear transcription factors. (3, 5, 6)
The effects of growth factor in the body
- Growth factors are proliferation regulators. Cells need growth factor to proliferate. Only a few cells can make it through without the growth factor.
- Growth factors regulate differentiation (both positive and negative). The actions of some type of growth factors have a lot to do with the development of the cells.
- They regulate cell migration and path finding.
- They also regulate the growth, survival, and death of cells. (4, 5)
Growth factor supplement
The body’s growth factor level can be affected by various bodily and health conditions. To supplement the body’s need for growth factor, various growth factor supplements were created.
It is important to supplement the body’s need for growth factor because it does not only stimulate cellular growth, but aids in various functions of the body. It plays a major role in cellular differentiation, hastens the healing process, and cellular proliferation, to name a few. (2)
There are many growth factor supplements today. The most popular ones include the following:
Human growth factor serum
It is a powerful nutritional supplement. Many bodybuilders and athletes take it because it can significantly enhance their physical performance, increase muscle mass, and improve their endurance and stamina.
As a matter of fact, the growth factor serum is one of the vital components of face cream. It also helps counteract the aging process.
How is it possible? Growth factor serum has a high level of epidermal growth factor. When you massage it in the skin, it will create a silky sensation. It expedites tissue regrowth and balances the moisture of the skin.
It also protects the skin from free radicals. It nourishes the skin and provides protection from cellular degradation. Growth factor serum is also one of the primary components of peeling treatments. (2, 3, 9)
Chlorella growth factor (CGF)
It is one of the most popular growth factor supplements today. It is derived from chlorella algae, which is considered a super food. It has anti-ageing, immune boosting, and detoxifying property. It hastens cellular repair. It makes you grow fast.
The growth ability of chlorella growth factor is what makes it one of the preferred supplements today. Kids grow faster and they become healthier when taking chlorella growth factor supplement on a day to day basis.
Take a look at the benefits of chlorella growth factor supplement:
- Chlorella growth factor plays a very important role in detoxification. It helps flush out harmful toxins from the body.
- It promotes cellular healing and repair. Damaged tissues will be able to bring back to its pre-damaged state.
- Chlorella growth factor increases growth spurts. A daily intake of chlorella growth factor promotes rapid growth in children.
- It counteracts the effect of aging. It improves the condition of the hair, nails, and skin.
- It boosts the body’s ability to fight diseases. It stimulated the production of interferons, a type of immune protein the body produced to combat pathogens.
- Chlorella growth factor improves the number of healthy bacteria in the gut. A regular intake of chlorella growth factor can help improve the digestive processes of the body.
- Chlorella growth factor boosts the body’s energy level. It improves the body’s metabolism by stimulating the production of enzymes, proteins, and energy. (6, 7, 8)
Growth factor as the primary component of skin creams
Growth factors are proteins that help regulate the growth, differentiation, and proliferation of cells under a controlled condition. They play a crucial role in maintaining a healthy skin structure. All cell types that make up the skin layers secrete growth factors including the epidermis and dermis.
Growth factors in the skin stimulate biochemical pathways to promote repair and regeneration of skin tissues. They facilitate collagen and elastic fiber formation, which makes the skin supple and soft. Skin care products containing growth factors reduce the formation of fine lines and wrinkles.
They even out pigmentation and age spots. They keep the skin smooth and tight. (1, 2, 10)
References:
- https://en.wikipedia.org
- www.sinobiological.com
- https://themedicalbiochemistrypage.org
- www.getgrowthfactor.com
- www.sciencedirect.com
- www.abmgood.com
- www.skinmedica.com
- www.growthfactor.com
- www.raybiotech.com
- Epidermal Growth Factor: Methods and Protocols edited by Tarun B. Patel, Paul J. Bertics
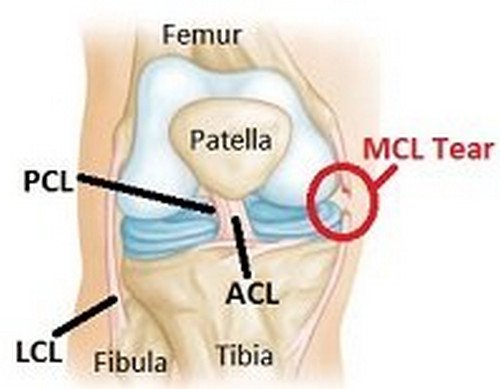
 Image 1: Anatomy of the knee joints.
Image 1: Anatomy of the knee joints.