What is Basal Ganglia?
The basal ganglia or basal nuclei are group of subcortical nuclei located at the base of the forebrain. They are significantly united with the cerebral cortex, thalamus, and brainstem. The basal ganglia play a major role in voluntary motor functions, procedural learning, routines or habits, and eye movements. They also have contributions in cognition and emotions [1].
Parts of the Basal Ganglia
1. Caudate Nucleus
This is where the complex or association loop of the basal ganglia traverses as it receives input from the association areas of the brain to transmit the information to the prefrontal cortex.
2. Putamen
This is where the motor loop of the basal ganglia traverses as it receives input from the sensorimotor cortex to transmit the information to the premotor area.
3. Globus Pallidus
Also known as pallidum or paleostriatum, it is the principal output structure of the basal ganglia.
4. Subthalamic Nucleus
It is a structure surrounded by the substantia nigra, thalamus, and internal capsules which has a role on action selection.
5. Substantia Nigra
Its name is derived from a Latin term meaning black substance. It is where dopamine resides. Dopamine is rich in neuromelanin which is rich in dark pigments, hence its name.
6. Nucleus accumbens
7. Olfactory Tubercle
-
Lentiform Nucleus = Putamen + Globus Pallidus
-
Striatum or Neostriatum = Caudate Nucleus + Putamen
-
This is the principal receptive structure of the basal ganglia.
-
Corpus Striatum = Neostriatum + Paleostriatum [2, 3, 4]
Blood Supply of the Basal Ganglia
The perforating branches of the anterior cerebral artery and recurrent arteries of Heubner supply the anterior and inferior heads of the caudate nucleus, anterior limb of the internal capsule, and parts of putamen and globus pallidus.
The anterior choroidal artery and perforating branches of the supraclinoid branch of the internal carotid artery go towards the middle of the brain to supply the medial part of globus pallidus.
The sphenoidal segment of middle cerebral artery supplies the body of the caudate nucleus, lateral globus pallidus, putamen, and dorsal internal capsule [3].
Photos of Anatomy of the Basal Ganglia: Where is it Located?

Picture 1: Structure of the Brain and Location of the Basal Ganglia
Image Source: neuroanatomyblog.tumblr.com

Picture 2: The Basal Ganglia
Image Source: upright-health.com

Picture 3: Parts of the Basal Ganglia
Image Source: commons.wikimedia.org

Picture 4: Relationship of the Basal Ganglia to the Thalamus and Ventricles
Parts of the basal ganglia are emphasized in bold letters.
Image Source: antranik.org

Picture 5: Blood Supply of the Basal Ganglia
Image Source: radiologyassistant.nl
What are the Functions of the Basal Ganglia?
- The basal ganglia allow you to automatically perform a learned motor behavior.
- From your motor memory, basal ganglia facilitates in preparing for motor action.
- It controls and modifies your movements.
- It is one of the brain structures that maintain posture.
- Basal ganglia play a role in memory retrieval [2].
Stroke Definition
Medically termed cerebrovascular disease or cerebrovascular accident (CVA), stroke is referred to any pathologic disturbance in the blood vessels of the brain causing some parts of it to be deprived of blood and oxygen, resulting to neurologic deficits and possibly death. It may be ischemic or hemorrhagic [5].

Picture 6: Hemorrhagic Stroke vs. Ischemis Stroke
Image Source: heart.arizona.edu
Risk Factors of Basal Ganglia Stroke
- Hypertension occurs in 90% of the cases.
- Moyamoya disease
- Chronic alcoholism
- Use of cocaine [3]
Signs and Symptoms of Bilateral or One-Sided Basal Ganglia Stroke
Cerebrovascular disease of the basal ganglia often shows motor dysfunctions. The severity of signs and symptoms depends on how extensive the damage is and which parts of the basal ganglia are specifically affected.
Limitation in Motor Activities
- Ataxia or inability to coordinate muscles
- Muscle weakness and rigidity
- Involuntary tremors
- Facial asymmetry
- Pocketing happens when the mouth or throat is affected. This means the foods are only chewed or held on one side of the mouth.
Impaired Sensation
The patient will not be able to normally feel stimuli as he had before the stroke. He may not be able to feel touch, pain, temperature, or pressure in a certain area of his body. He may not even know which body part is being touched.
Speech Problems
- Nonfluent Aphasia
The patient has a problem with speaking his mind. What is in his mind is not completely what comes out of his mouth. There are missing words and incomplete sentences. He finds it difficult to speak.
- Fluent Aphasia
The patient does not find it hard to speak. He speaks fluently and in complete sentences. The problem here is the words itself. His sentences are jumbled words that have no meaning altogether. What the patient wants to say is completely different from what comes out of his mouth. The statements do not make sense at all.
- Global Aphasia
The patient cannot speak nor understand words.
Changes in the Eyes
- Trouble looking upwards or sidewards
- Loss of visual field in some areas
- Pupils are asymmetrical in size
Personality Changes
- Depression
- Inappropriate affect
- Inappropriate emotions
- Rage
- Frustration
- Nervousness
- Avolition or lack of motivation [6]
Right Basal Ganglia Stroke
- Anosognosia is a state wherein the patient is not aware or unable to perceive the severity of his deficit. This is frequent among patients who had right-sided hemispheric stroke, affecting the right middle cerebral artery, which supplies parts of the basal ganglia.
- Left-side neglect happens in patients who had basal ganglia stroke on the right side of his brain. The patient will unconsciously neglect or ignore anything that is on his left side. He only pays attention on what’s on the right side of his body. He may even have trouble moving his body parts to the left.
- Infarction and haemorrhage of the right anterior choroidal and lenticulostriate arteries put the basal ganglia and internal capsule into the picture. There will be visuospatial hemineglect, constructional apraxia, motor impersistence, and anosognosia.
- Infarction of right anterior choroidal artery does not cause impairment in memory [6, 7].
Left Basal Ganglia Stroke
- Apathy, meaning lack of interest or concern as manifested by inactivity, occurs after the occurrence of lesion on the left basal ganglia.
- Infarction of left anterior choroidal artery may cause impairment in memory.
- Stroke in the left basal ganglia is associated with post-operative major depression. There is a study saying that major depression is twice likely to occur in left basal ganglia stroke than the right. It was also said that depressive disorder is more likely to occur in strokes located in the basal ganglia than in the thalamus, so as with middle cerebral artery than in posterior blood vessels [7, 8].
Neurologic Disorders associated with Basal Ganglia Stroke
Recurrent Artery of Heubner Syndrome
Recurrent artery of Heubner or medial striate artery is a branch of the anterior cerebral artery. Infarction of this blood vessel results to weakness of the face and arm contralateral to the affected side of the brain. Cognitive and behavioural abnormality may also be observed. The infarcted parts include the anterior part of the basal ganglia, inferior frontal lobe, and anterior internal capsule [2].
Thalamic Syndrome
A group of signs and symptoms including sensory loss, pain, dysesthesia, choreoathetosis, tremor, and hemiparesis occur if thalamogeniculate artery is occluded. Hemiballismus is an additional symptom if the subthalamic nucleus and globus pallidus are affected.
Transient Choreoathetosis
It comes from the root words “chorea” which is an uncontrollable, rapid movement and “athetosis” meaning twisting and wiggling movement of the hands and feet. During prolonged activity, choreoathetosis seems to trigger ischemia of the anterior basal ganglia [5].
Treatment for Basal Ganglia Stroke

Picture 7: Warning Signs of Stroke
Image Source: dhhs.ne.gov
Remember the image above. If there is someone with you and they manifest these signs, you better act fast and rush to the hospital as quick as you can. You may be saving that person’s life.
Once the patient gets into the emergency room, the physician provides measures to dissolve the clot and prevent further clot formation through blood thinning medications. Fluids are administered and vital signs are stabilized. Lowering the blood pressure and intracranial pressure is extremely important.
If not treated by medications, the patient undergoes into emergency surgery to remove the cause itself as it is fatal to the patient if the brain does not get enough blood and oxygen. Time is of the essence because the longer the brain becomes deprived, the higher the chance of disability and mortality.
After recovery, the patient gets into different kinds of therapies, depending on severity of damage the stroke. He signs into physical therapy, speech therapy, occupational therapy, and others which may help him regain his former functions. The goal here is to optimize the patient’s capabilities so he can live his life to the fullest.
It is also very important to prevent it from happening again by stabilizing the blood pressure and avoiding all the risk factors.
Prognosis of Basal Ganglia Stroke
- Approximately 33% of all stroke cases are deadly. Prognosis depends on the underlying cause, how extensive it is, how soon it was medically treated, size and location of the lesion, degree of deficit, and age of the patient.
- The chance of death for patients with hemorrhagic stroke is 70% while for ischemic stroke, mortality is lower which is 25%. However, reoccurrence of ischemic stroke is 5-15% every year [9].
- Patients who had stroke confined to the basal ganglia have smaller lesions but slower initial recovery time compared to those who had stroke on the cerebral cortex. Although the recovery was gradual during early rehabilitation stage, it significantly progresses towards the end. Compared to patients who had stroke on cerebral cortex, those who had stroke on basal ganglia had a greater overall recovery [10].
- The earlier the stroke was recognized and treated, the better the prognosis. The greater the Glasgow coma scale (GCS) score of the patient, the better the prognosis.
Prevention of Stroke
Any forms of CVA are dangerous to face. The best way to never experience stroke is prevention. In order to do that, risk factors (as enumerated in the earlier section of this article) to stroke should be eliminated.
The physician’s prudence in the identification of early signs of stroke such as transient ischemic attack (TIA), carotid artery stenosis, and atrial fibrillation is a very important element in saving a patient’s life [5].
References:
- Basal Ganglia accessed on http://en.wikipedia.org/wiki/Basal_ganglia
- Afifi AK & Bergman RA, Functional Neuroanatomy: Text and Atlas 2nd edition, McGraw-Hill 2005
- Caplan LR, Stroke Syndromes 3rd edition, Cambridge University Press, 2012, p 509
- Greenstein B & Greenstein A, Color Atlas of Neuroscience, Thieme 2000 , p 186
- Ropper AH & Samuels MA, Adams & Victor’s Principles of Neurology 9th edition, McGraw-Hill Companies Inc. 2009
- Basal Ganglia Stroke accessed on https://patienteducation.osumc.edu/Documents/BasalGangliaStroke.pdf
- Godefroy O, The Behavioral and Cognitive Neurology of Stroke, Cambridge University Press 2013, pp 37-38
- Schaller B, State-of-the-Art Imaging in Stroke, Nova Publishers 2007, p 80
- Lindsay KW et al, Neurology and Neurosurgery Illustrated 3rd edition, Churchill Livingstone 1997, pp 236-237
- Barnes MP et al, Recovery after Stroke, Cambridge University Press 2005, p 162


















 Picture : Oral Lymphoepithelial Cyst or Cystic Ectopic Lymphoid Tissue
Picture : Oral Lymphoepithelial Cyst or Cystic Ectopic Lymphoid Tissue
























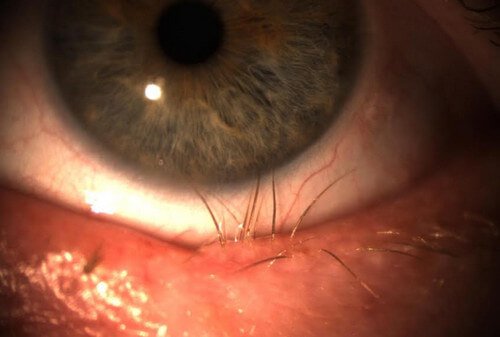

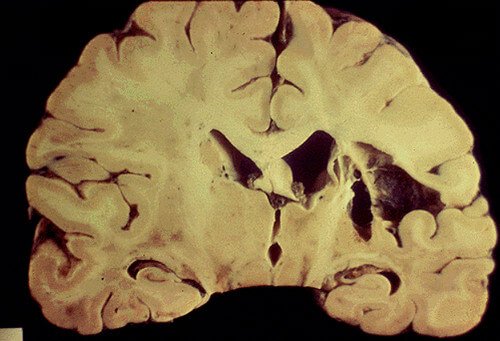

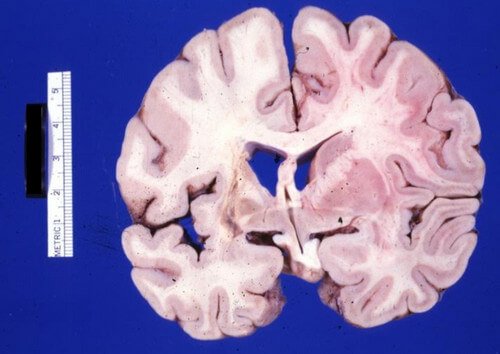




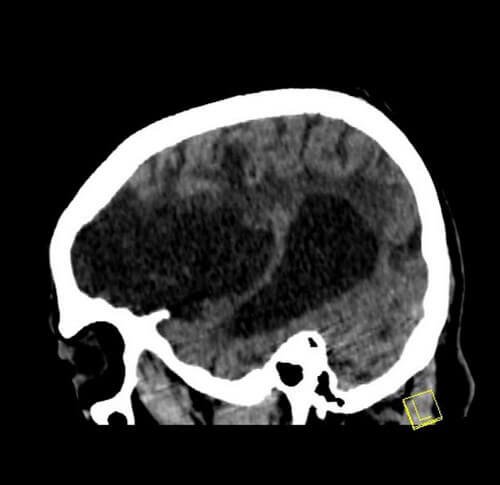
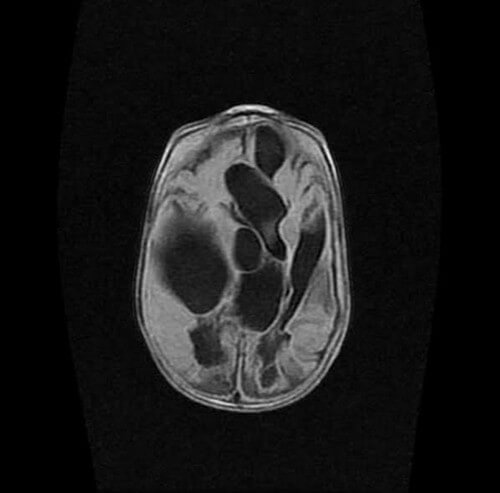

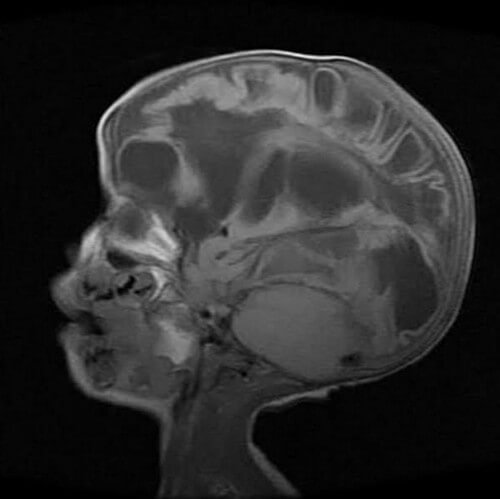
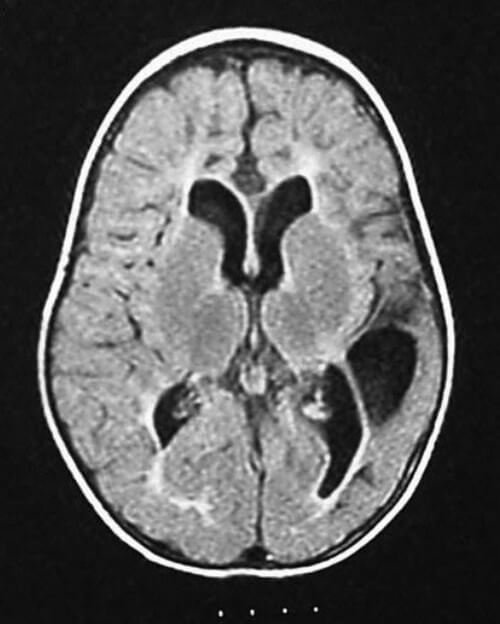

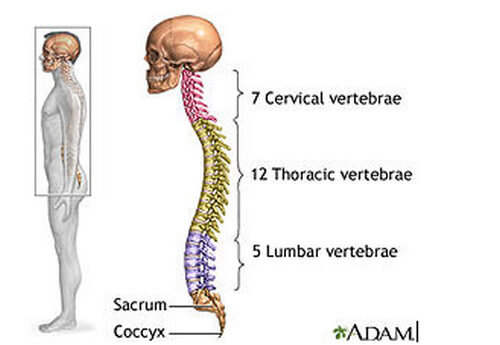



















 Image 1: Fordyce spots on upper lip
Image 1: Fordyce spots on upper lip Picture 2 : Fordyce spots located on or around the lips (mouth)
Picture 2 : Fordyce spots located on or around the lips (mouth) In this image, you can see the difference between natural Fordyce spots on the penile shaft as well as one that was irritated by the patient “picking” at the spot.
In this image, you can see the difference between natural Fordyce spots on the penile shaft as well as one that was irritated by the patient “picking” at the spot. This image also shows the natural appearance of Fordyce spots on the penile shaft.
This image also shows the natural appearance of Fordyce spots on the penile shaft.





